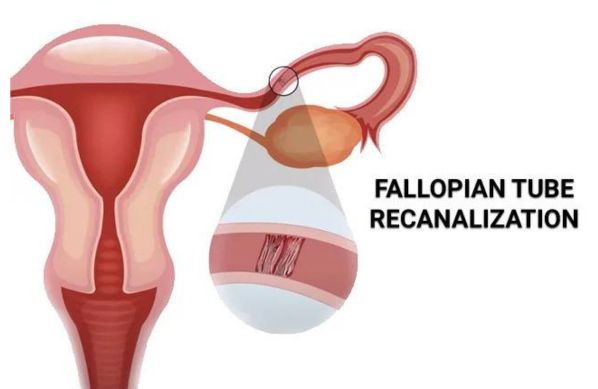
Fallopian Tube Recanalization is a minimally invasive procedure used to treat blockages in the fallopian tubes, one of the common causes of infertility in women. By opening the blocked tubes, this procedure helps restore the natural pathway for the egg and sperm to meet, increasing the chances of conception. Fallopian Tube Recanalization is typically performed as an outpatient procedure and can be a suitable option for women with certain types of tubal blockages. Here are some key aspects of Fallopian Tube Recanalization:
Indications for Fallopian Tube Recanalization: Fallopian Tube Recanalization is indicated for women experiencing infertility due to blockages in the fallopian tubes. These blockages are commonly caused by:
Scar Tissue or Adhesions: Resulting from prior infections, such as pelvic inflammatory disease (PID).
Mucus or Debris: Small blockages in the tube that can obstruct egg and sperm passage.
Previous Tubal Infections or Surgeries: Surgical procedures or infections that may leave residual blockages.
Pre-Procedure Assessment and Counseling: Before undergoing recanalization, a comprehensive evaluation is performed, including medical history, imaging studies such as hysterosalpingography (HSG), and any additional fertility testing if needed. Counseling is a key part of the process, as it helps the patient understand the recanalization procedure, its benefits, and any associated risks. This ensures the patient is fully informed and prepared for the treatment.
Diagnostic Imaging and Confirmation of Blockage: Fallopian Tube Recanalization usually starts with a diagnostic imaging study, often a hysterosalpingogram (HSG), to confirm the location and nature of the blockage. This imaging provides real-time visualization of the fallopian tubes and helps guide the procedure.
The Recanalization Procedure: The recanalization procedure is minimally invasive and typically takes about 30 to 60 minutes. Under local or mild sedation, a thin catheter is inserted through the cervix into the uterus, and a contrast dye is injected to highlight the fallopian tubes. A smaller catheter or wire is then used to gently clear the blockage, allowing the fallopian tube to reopen. This technique minimizes trauma to the surrounding tissue.
Post-Procedure Monitoring: After the procedure, patients are monitored briefly and may experience mild cramping or spotting. Most can return to their daily activities within 24 hours. Follow-up imaging or additional testing may be recommended in some cases to ensure the tubes remain open.
Emotional and Psychological Support: Dealing with infertility and undergoing treatments can be emotionally challenging for many women. Psychological support, including counseling services and support groups, may be beneficial for coping with the stress and anxiety related to fertility treatment.
Benefits of Minimally Invasive Treatment: Fallopian Tube Recanalization offers several benefits over more invasive surgical options. It is performed on an outpatient basis, has a short recovery time, and allows patients to resume normal activities quickly. By directly targeting blockages, it provides a high success rate for opening the tubes without the need for traditional surgery.
Risks and Considerations: Although recanalization is generally safe, potential risks include infection, injury to the fallopian tube, or re-blockage over time. Healthcare providers discuss these risks with the patient to ensure informed decision-making. In some cases, alternative fertility treatments may be recommended if recanalization is not feasible.
Fallopian Tube Recanalization is a valuable treatment option for women with blocked fallopian tubes, providing a minimally invasive path to potentially restoring fertility. Through precise techniques and supportive care, recanalization offers a hopeful solution for women seeking to conceive naturally.
Dr. Ravneet Kaur Offers a comprehensive range of obstetrics and gynaecology treatments, utilizing advanced techniques and personalized care to support patients on their journey to reproductive health and wellness.

High-risk pregnancy care refers to specialized medical services aimed at monitoring and managing pregnancies with increased risks due to various factors.

Painless delivery, also known as epidural analgesia, refers to the use of pain relief methods during labor to help women manage the discomfort of childbirth.

Intrapartum fetal monitoring, commonly referred to as Toco-Cardio Graphy (CTG), is a crucial method used during labor to assess the well-being of the fetus.

Recurrent pregnancy loss (RPL) refers to the occurrence of two or more consecutive miscarriages, and it affects a small percentage of women trying to conceive.

Menopausal treatment focuses on managing the symptoms and health risks associated with menopause, which marks the end of a woman's reproductive years.

Laparoscopically Assisted Vaginal Hysterectomy (LAVH) is a minimally invasive surgical procedure used to remove the uterus.

Laparoscopy and hysteroscopy are minimally invasive surgical procedures used to diagnose and treat various gynaecology conditions.
In Vitro Fertilization (IVF) is a sophisticated assisted reproductive technology (ART) that enables individuals or couples facing fertility challenges to conceive a child.

Intrauterine Insemination (IUI) is a widely used assisted reproductive technology (ART) that involves placing sperm directly into a woman’s uterus during her ovulation period.

Intracytoplasmic Sperm Injection (ICSI) is a specialized form of assisted reproductive technology (ART) used to address male infertility issues.

