
High-risk pregnancy care refers to specialized medical services aimed at monitoring and managing pregnancies with increased risks due to various factors. These factors can include maternal health conditions, fetal anomalies, advanced maternal age, or previous pregnancy complications. High-risk pregnancy care is typically provided by obstetricians with expertise in high-risk obstetrics, maternal-fetal medicine specialists, and a multidisciplinary team of healthcare professionals. Here are some key aspects of high-risk pregnancy care:
Diagnosis and Assessment: High-risk pregnancy care begins with thorough assessments to identify any potential risks. This includes comprehensive evaluations such as ultrasounds, blood tests, and screenings for conditions like gestational diabetes and preeclampsia. Early identification of risks is crucial for effective management throughout the pregnancy.
Individualized Care Plans: healthcare providers develop personalized care plans tailored to the mother’s and fetus's specific needs. These plans may include increased monitoring, medication management, dietary recommendations, and lifestyle modifications to ensure the best possible outcomes.
Continuous Monitoring: Women with high-risk pregnancies require more frequent prenatal visits for close monitoring of both maternal and fetal health. This may involve regular ultrasounds, fetal heart rate monitoring, and other diagnostic tests to track the pregnancy’s progress and identify any emerging complications.
Education and Counseling: Patient education is a vital aspect of high-risk pregnancy care. Healthcare providers educate patients about their condition, potential risks, and self-care strategies. They offer counseling on signs of complications, nutrition, exercise, and emotional support, empowering women to manage their pregnancies effectively.
Multidisciplinary Collaboration: High-risk pregnancy care often involves a team approach, with obstetricians, maternal-fetal medicine specialists, nurses, nutritionists, and mental health professionals collaborating to provide comprehensive care. This team coordinates efforts to address the diverse needs of both the mother and fetus.
Preconception Counseling: For women identified as high-risk before conception, preconception counseling is essential. Healthcare providers discuss strategies to optimize maternal health and minimize risks before pregnancy, which may include managing chronic conditions and lifestyle changes.
Psychological Support Pregnancy can be stressful, especially for women facing high-risk factors. Psychological support and counseling services may be integrated into care to address anxiety, depression, and other emotional challenges, promoting mental well-being throughout the pregnancy journey.
Delivery Planning: Planning for delivery is a critical aspect of high-risk pregnancy care. Healthcare providers discuss the safest delivery options, including the possibility of cesarean delivery, and prepare for any special interventions needed during labor and delivery to ensure the safety of both mother and baby.
Postpartum Care: After delivery, high-risk pregnancy care continues with close monitoring of maternal and newborn health. Healthcare providers assess for any complications, provide breastfeeding support, and offer resources for physical and emotional recovery during the postpartum period.
High-risk pregnancy care is essential for ensuring the health and well-being of both mother and baby. By providing comprehensive monitoring, individualized care, and support, healthcare providers aim to reduce risks, improve outcomes, and enhance the overall pregnancy experience for women facing high-risk factors.
Dr. Ravneet Kaur Offers a comprehensive range of obstetrics and gynaecology treatments, utilizing advanced techniques and personalized care to support patients on their journey to reproductive health and wellness.

High-risk pregnancy care refers to specialized medical services aimed at monitoring and managing pregnancies with increased risks due to various factors.

Painless delivery, also known as epidural analgesia, refers to the use of pain relief methods during labor to help women manage the discomfort of childbirth.

Intrapartum fetal monitoring, commonly referred to as Toco-Cardio Graphy (CTG), is a crucial method used during labor to assess the well-being of the fetus.

Recurrent pregnancy loss (RPL) refers to the occurrence of two or more consecutive miscarriages, and it affects a small percentage of women trying to conceive.

Menopausal treatment focuses on managing the symptoms and health risks associated with menopause, which marks the end of a woman's reproductive years.

Laparoscopically Assisted Vaginal Hysterectomy (LAVH) is a minimally invasive surgical procedure used to remove the uterus.

Laparoscopy and hysteroscopy are minimally invasive surgical procedures used to diagnose and treat various gynaecology conditions.
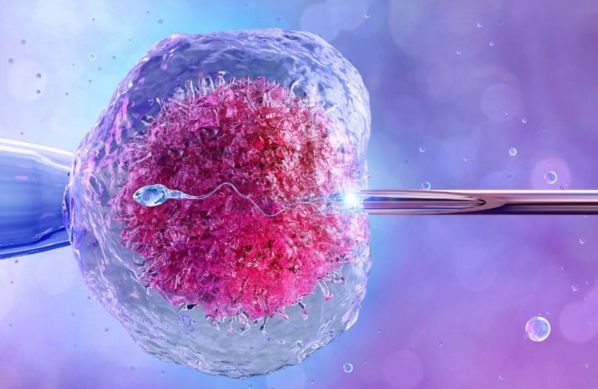
In Vitro Fertilization (IVF) is a sophisticated assisted reproductive technology (ART) that enables individuals or couples facing fertility challenges to conceive a child.

Intrauterine Insemination (IUI) is a widely used assisted reproductive technology (ART) that involves placing sperm directly into a woman’s uterus during her ovulation period.

Intracytoplasmic Sperm Injection (ICSI) is a specialized form of assisted reproductive technology (ART) used to address male infertility issues.

