
Laparoscopically Assisted Vaginal Hysterectomy (LAVH) is a minimally invasive surgical procedure used to remove the uterus. It combines the advantages of both laparoscopic and vaginal surgery, offering a less invasive alternative to traditional abdominal hysterectomy. LAVH is often recommended for conditions such as fibroids, endometriosis, uterine prolapse, or chronic pelvic pain. The procedure involves the use of a laparoscope to assist in detaching the uterus, which is then removed through the vagina. Here are some key aspects of Laparoscopically Assisted Vaginal Hysterectomy (LAVH):
Indications for LAVH: LAVH is typically performed for conditions that affect the uterus and have not responded to non-surgical treatments. These include fibroids, abnormal uterine bleeding, endometriosis, chronic pelvic pain, and uterine prolapse. LAVH is also considered in cases of precancerous conditions or early-stage uterine cancer.
Surgical Procedure: LAVH begins with small incisions in the abdomen through which a laparoscope (a thin, lighted tube with a camera) and surgical instruments are inserted. The laparoscope allows the surgeon to view the pelvic organs and safely detach the uterus from surrounding tissues. Once detached, the uterus is removed through the vaginal canal. The procedure may also involve the removal of the fallopian tubes and ovaries, depending on the patient’s condition and health goals.
Benefits of LAVH: LAVH offers several benefits over traditional abdominal hysterectomy. These include smaller incisions, less post-operative pain, a shorter hospital stay, and a quicker recovery period. Additionally, the laparoscopic approach provides the surgeon with a clear view of the pelvic area, reducing the risk of complications and allowing for precise removal of the uterus.
Preoperative Evaluation and Counseling: Before undergoing LAVH, patients undergo a thorough preoperative evaluation, which includes a physical examination, imaging studies (such as ultrasound or MRI), and blood tests. Healthcare providers also offer counseling to explain the procedure, discuss the risks and benefits, and address any concerns or questions the patient may have.
Anesthesia and Pain Management: LAVH is performed under general anesthesia, meaning the patient is completely unconscious during the surgery. Pain management is an essential part of the procedure, and patients are given medications to manage post-operative discomfort. Minimally invasive surgery like LAVH typically results in less post-operative pain compared to open surgery.
Recovery and Postoperative Care: Recovery from LAVH is generally quicker than from traditional hysterectomy. Most patients can go home within 24 to 48 hours after the surgery and return to normal activities within a few weeks. Postoperative care includes pain management, wound care, and follow-up visits to ensure proper healing. Patients are advised to avoid heavy lifting and strenuous activities during the initial recovery period.
Minimizing Complications: As with any surgical procedure, there are risks associated with LAVH, including infection, bleeding, or injury to surrounding organs like the bladder or bowel. However, the laparoscopic approach minimizes these risks due to the precision of the surgery. Healthcare providers take precautions to prevent complications and monitor patients closely during recovery.
Psychological and Emotional Support: Undergoing a hysterectomy can be an emotional experience for many women, especially those who are dealing with infertility or concerns about their body image. Emotional and psychological support is provided as part of the treatment process, with counseling services available to help patients cope with the physical and emotional aspects of the surgery.
Laparoscopically Assisted Vaginal Hysterectomy (LAVH) offers a less invasive, safer alternative to traditional hysterectomy, providing faster recovery, reduced pain, and improved surgical precision. By combining laparoscopic technology with vaginal surgery, LAVH allows for a more efficient and effective removal of the uterus, helping women manage a wide range of gynecological conditions with minimal disruption to their lives.
Dr. Ravneet Kaur Offers a comprehensive range of obstetrics and gynaecology treatments, utilizing advanced techniques and personalized care to support patients on their journey to reproductive health and wellness.

High-risk pregnancy care refers to specialized medical services aimed at monitoring and managing pregnancies with increased risks due to various factors.

Painless delivery, also known as epidural analgesia, refers to the use of pain relief methods during labor to help women manage the discomfort of childbirth.

Intrapartum fetal monitoring, commonly referred to as Toco-Cardio Graphy (CTG), is a crucial method used during labor to assess the well-being of the fetus.

Recurrent pregnancy loss (RPL) refers to the occurrence of two or more consecutive miscarriages, and it affects a small percentage of women trying to conceive.

Menopausal treatment focuses on managing the symptoms and health risks associated with menopause, which marks the end of a woman's reproductive years.

Laparoscopically Assisted Vaginal Hysterectomy (LAVH) is a minimally invasive surgical procedure used to remove the uterus.

Laparoscopy and hysteroscopy are minimally invasive surgical procedures used to diagnose and treat various gynaecology conditions.
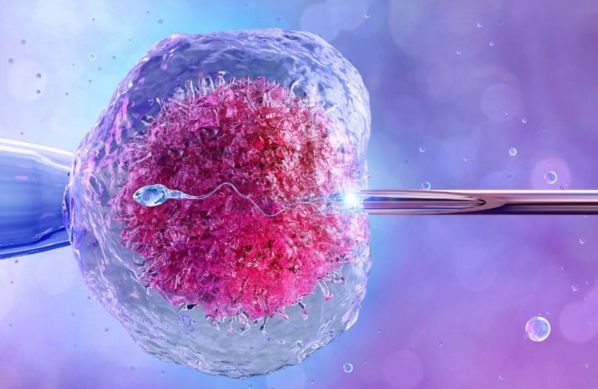
In Vitro Fertilization (IVF) is a sophisticated assisted reproductive technology (ART) that enables individuals or couples facing fertility challenges to conceive a child.

Intrauterine Insemination (IUI) is a widely used assisted reproductive technology (ART) that involves placing sperm directly into a woman’s uterus during her ovulation period.

Intracytoplasmic Sperm Injection (ICSI) is a specialized form of assisted reproductive technology (ART) used to address male infertility issues.

